Mortality prediction based on CURB-65 criteria
Community-acquired pneumonia (CAP) in an elderly patient carries a variable mortality risk, which ranges from less than 1% to over 50%. Key factors influencing the outcome include existing comorbidities, level of consciousness, clinical parameters, and laboratory findings.
Over the years, several scoring systems have been developed to predict risk levels and guide patient management.
We can use one of these scoring systems to attempt a prognosis in the coming days.
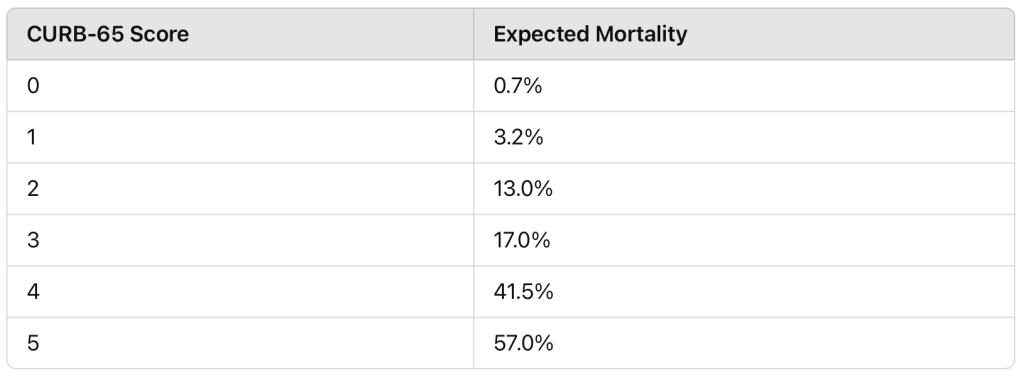
One of the most accurate is the Pneumonia Severity Index (PSI/PORT score), but it cannot be used due to a lack of data on the Pope’s medical history and recent laboratory tests. However, a score can be estimated using the CURB-65 scale, which is fairly effective in predicting 30-day mortality. The score ranges from 0 to 5, with one point assigned for each parameter.
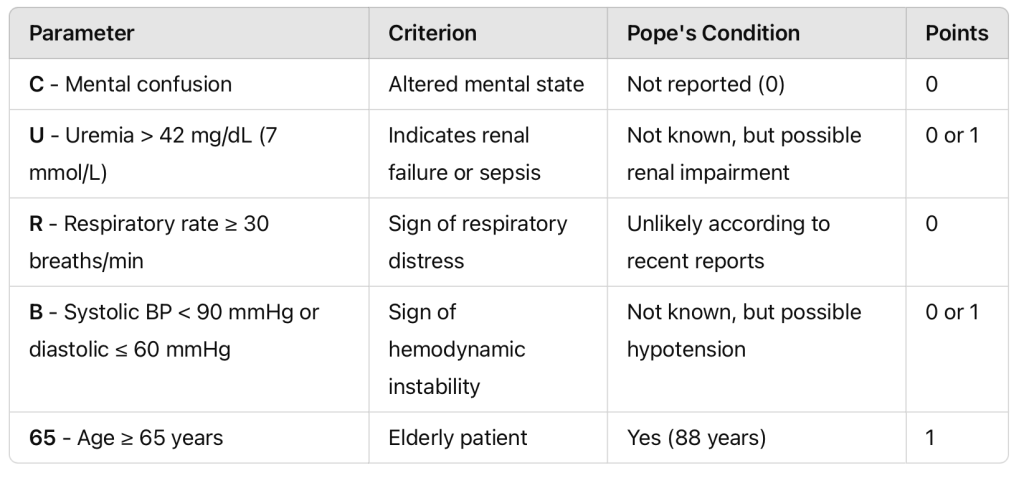
The only risk factor that the Pope certainly meets is age (+1 point). Based on the latest press releases, there is no reason to believe he is experiencing mental confusion: he regularly eats, speaks, and reads newspapers (score 0). He is also described as calm and “self-ventilated”; any episodes of tachypnea or hyperventilation would have been reported (score 0). There is no information regarding blood urea nitrogen or blood pressure (each ranging from 0 to 1).
His CURB-65 score is estimated between 1 and 3, with 2 being the minimum threshold for hospitalization and 3-4 for intensive care.
“Defining community-acquired pneumonia severity on presentation to hospital: an international derivation and validation study”
Assuming there has been no filtering of information by the Vatican press office, the estimated short-term mortality risk ranges between 3.2% and 17.0%.
It is important to emphasize that the Pope’s condition remains highly complex and could deteriorate at any moment. Multiple pathogens resistant to antibiotic therapy are present in his airways. Additionally, his immune system is weakened due to ongoing corticosteroid treatment, aimed at reducing inflammation and improving respiratory function. Cortisone is a double-edged sword, used only in severe pneumonia cases: it limits damage and fluid accumulation in the alveoli but also “reduces the host’s defenses, promoting secondary bacterial infections. Constant reassessment of antibiotic therapy is required” (Source: Professor of Infectious Diseases Massimo Andreoni, ANSA).
If the infection prevails, bacteria could enter the bloodstream within 24 hours, leading to sepsis. This could rapidly progress to fatal multi-organ failure within days.
Another possible outcome is acute respiratory distress syndrome (ARDS), causing fluid-filled lungs and requiring mechanical ventilation. In this case, mortality could rise as high as 50%.
Estimating a precise mortality risk remains speculative. The situation must be monitored daily, since there’s no crystal ball in medicine.
VERSIONE ITALIANA: https://zetaluiss.it/wp-admin/post.php?post=217371&action=edit

